MBBS, MD’Clinical Ordinatura (Cardiology)
FACC, FICC, Fellowship in Intervention Cardiology
Adult and Paediatric Intervention Cardiologist
MBBS, MD’Clinical Ordinatura (Cardiology)
FACC, FICC, Fellowship in Intervention Cardiology
Adult and Paediatric Intervention Cardiologist
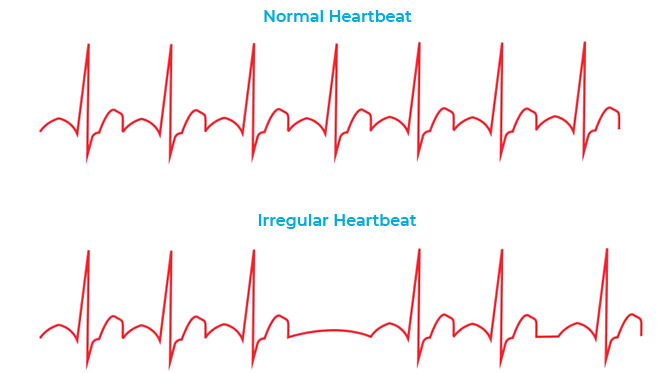
Your heart is hard at work as it pumps blood and nutrients throughout your body. You can sometimes hear it or even feel it as it beats at a steady pace. It’s got an even, reliable rhythm that’s controlled by your body’s own electrical system. When that system has issues, though, you get a change in your heart’s rhythm that’s called arrhythmia.If you have an arrhythmia, it doesn’t necessarily mean you’ve got heart disease. There are many things that can cause your heart to flutter.
It’s possible to have a random arrhythmia even if your heart is healthy. If you do, talk to your doctor. Arrhythmias are caused by:
A typical heart will beat at 60 to 100 times per minute. It can beat faster if you need it to during exercise or in a stressful situation. It can slow down while you sleep. Your heart is used to slowing down and speeding up. That’s normal.
There’s a node in the upper right section of your heart that monitors your body’s need for blood. It’s called the sinoatrial (SA) or sinus node, and it acts like a natural pacemaker. It’s the main control and source of each heartbeat. It can speed up your heart rate when you need it, like when you exercise or get sick, or even when you feel happy. Your SA node sends out electrical impulses across the heart. These cause the chambers to contract at specific times, causing a heartbeat.
Doctors classify arrhythmias not only by where they originate (atria or ventricles) but also by the speed of heart rate they cause:
Not all tachycardias or bradycardias mean you have heart disease. For example, during exercise it’s normal to develop a fast heartbeat as the heart speeds up to provide your tissues with more oxygen-rich blood. During sleep or times of deep relaxation, it’s not unusual for the heartbeat to be slower.
Tachycardias in the atria
Tachycardias originating in the atria include:
The chaotic electrical signals bombard the AV node, usually resulting in an irregular, rapid rhythm of the ventricles. Atrial fibrillation may be temporary, but some episodes won’t end unless treated.
Atrial fibrillation may lead to serious complications such as stroke.
Tachycardias in the ventricles
Tachycardias occurring in the ventricles include:
Most people who experience ventricular fibrillation have an underlying heart disease or have experienced serious trauma, such as being struck by lightning.
You can be born with a genetic mutation that puts you at risk of long QT syndrome. In addition, several medications may cause long QT syndrome. Some medical conditions, such as congenital heart defects, may also cause long QT syndrome.
Bradycardia -A slow heartbeat
In addition, certain medications used to treat other conditions, such as high blood pressure, may lower your heart rate. However, if you have a slow heart rate and your heart isn’t pumping enough blood, you may have one of several bradycardias, including:
Depending on the location and type of block, the impulses between the upper and lower halves of your heart may be slowed or blocked. If the signal is completely blocked, certain cells in the AV node or ventricles can make a steady, although usually slower, heartbeat.
Some blocks may cause no signs or symptoms, and others may cause skipped beats or bradycardia.
You may have noticed your heart racing, a fluttering in your chest, or a sensation that your heart skipped a beat. If this happens once or infrequently with no other symptoms; it’s usually not serious. Talk to us about your questions and concerns. If you get treatment and it doesn’t help, make sure to let us know as soon as you can. If you have any of the following symptoms, call us at +91 9591991809 right away:
To diagnose a heart arrhythmia, your doctor will review your symptoms and your medical history and conduct a physical examination. Your doctor may ask about – or test for – conditions that may trigger your arrhythmia, such as heart disease or a problem with your thyroid gland. Your doctor may also perform heart-monitoring tests specific to arrhythmias. These may include:
In addition, your cardiologist can use the electrodes to stimulate your heart to beat at rates that may trigger — or halt — an arrhythmia. This allows your doctor to see the location of the arrhythmia and what may be causing it
If you need treatment, the kind you get will depend on your case. You might need medication or surgery. Treatment for heart arrhythmias also may involve use of an implantable device:
If a pacemaker detects a heart rate that’s abnormal, it emits electrical impulses that stimulate your heart to beat at a normal rate.
An ICD is a battery-powered unit that’s implanted under the skin near the collarbone — similar to a pacemaker. One or more electrode-tipped wires from the ICD run through veins to the heart. The ICD continuously monitors your heart rhythm.
If it detects an abnormal heart rhythm, it sends out low- or high-energy shocks to reset the heart to a normal rhythm. An ICD doesn’t prevent an abnormal heart rhythm from occurring, but it treats it if it occurs.