Heart valve disease occurs when the heart valves do not work the way they should.
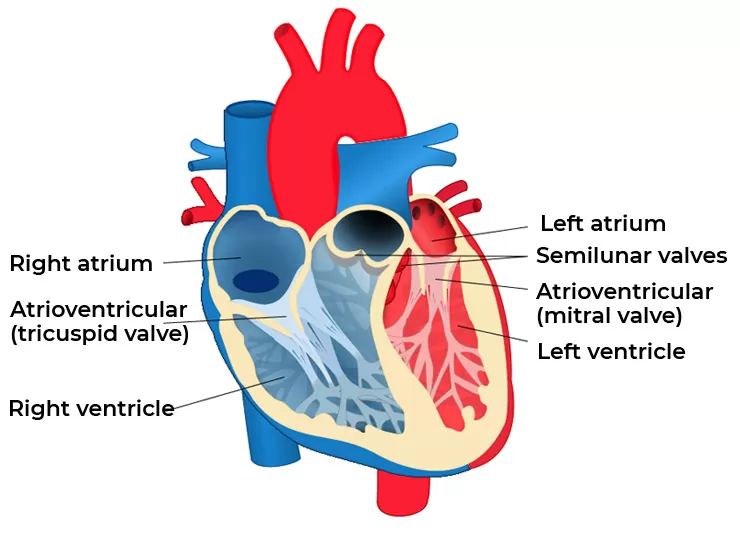
Your heart valves lie at the exit of each of your four heart chambers and maintain one-way blood flow through your heart. The four heart valves make sure that blood always flows freely in a forward direction and that there is no backward leakage. Blood flows from your right and left atria into your ventricles through the open tricuspid and mitral valves. When the ventricles are full, the tricuspid and mitral valves shut. This prevents blood from flowing backward into the atria while the ventricles contract. As the ventricles begin to contract, the pulmonic and aortic valves are forced open and blood is pumped out of the ventricles.
Blood from the right ventricle passes through the open pulmonic valve into the pulmonary artery, and blood from the left ventricle passes through the open aortic valve into the aorta and the rest of the body. When the ventricles finish contracting and begin to relax, the aortic and pulmonic valves shut. These valves prevent blood from flowing back into the ventricles. This pattern is repeated over and over with each heartbeat, causing blood to flow continuously to the heart, lungs, and body.
There are several types of heart valve disease:
Heart valve disease can develop before birth (congenital) or can be acquired sometime during one’s lifetime. Sometimes, the cause of valve disease is unknown.
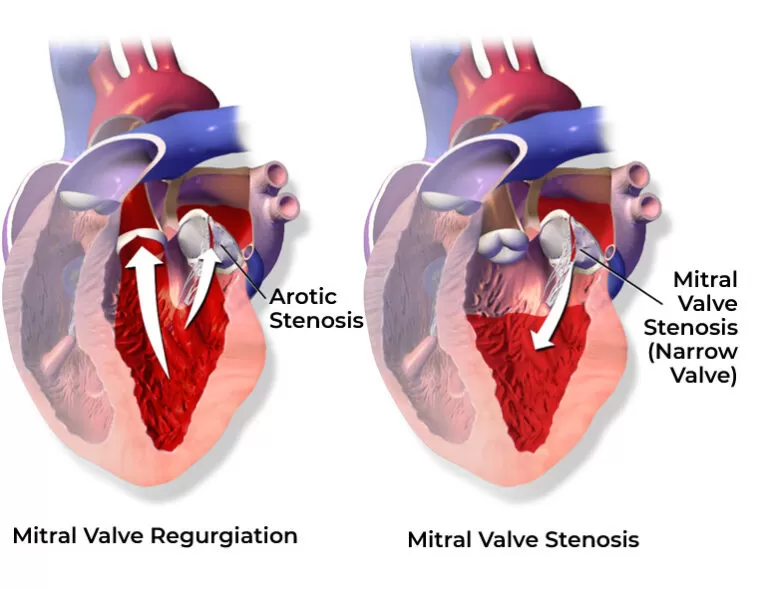
There are many changes that can occur to the valves of the heart. The chordae tendinae or papillary muscles can stretch or tear; the annulus of the valve can dilate (become wide); or the valve leaflets can become fibrotic (stiff) and calcified.
Other causes of valve disease include: coronary artery disease, heart attack, cardiomyopathy (heart muscle disease), syphilis (a sexually transmitted disease), high blood pressure, aortic aneurysms, and connective tissue diseases. Less common causes of valve disease include tumors, some types of drugs, and radiation.
Symptoms of heart valve disease can include but not limited to shortness of breath and/or difficulty catching your breath. You may notice this most when you are active (doing your normal daily activities) or when you lie down flat in bed. You may need to sleep propped up on a few pillows to breathe easier.
Symptoms of heart valve disease do not always relate to the seriousness of your condition. You may have no symptoms at all and have severe valve disease, requiring prompt treatment. Or, as with mitral valve prolapse, you may have noticeable symptoms, yet tests may show the valve leak is not significant.
our heart doctor can tell if you have heart valve disease by talking to you about symptoms, performing a physical exam, and performing other tests.During a physical exam, the doctor will listen to your heart to hear sounds the heart makes as the valves open and close. A murmur is a swishing sound made by blood flowing through a stenotic or leaky valve. A doctor can also tell if the heart is enlarged or if your heart rhythm is irregular. The doctor will listen to the lungs to hear if you are retaining fluid there, which shows the heart is not able to pump as well as it should. By examining your body, the doctor can find clues about circulation and the functioning of other organs. After the physical exam, the doctor may order diagnostic tests.
These may include:
By conducting some or all of these tests over time, your doctor can also see the progress of valve disease. This will help him or her make decisions about treatment.